ERCP Overview

What is Colon and Rectal Cancer Screening?
July 1, 2021
World Hepatitis Day 2021: Know about the Myths and Facts
July 20, 2021Endoscopy is the examination of an internal body part with an instrument called an endoscope. Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that uses X-ray to view the patient's bile and pancreatic ducts
The functions of the common bile duct and the pancreatic duct are to drain the gallbladder, liver, and pancreas; the two main ducts convey the bile and the pancreatic juice through the papilla into the duodenum (the first part of the small intestine). The most common reason why someone would need an ERCP is because of a blockage of one of these ducts (often due to gallstones). Generally, prior to ERCP blood tests and noninvasive imaging tests such as ultrasound, computed tomographic (CT) scan or magnetic resonance imaging (MRI) were performed.
The endoscopist (a doctor who has special training in the use of endoscopes) will examine the bile and/or pancreatic ducts, looking for abnormalities such as blockages, irregularity in the tissue, problems with the flow of bile or pancreatic fluid, stones, or tumors. If a problem is found, the endoscopist can often perform a procedure to repair or improve the condition; as a result, ERCP has replaced surgery in most patients with common bile duct and pancreatic disease.
Many patients who need ERCP are hospitalized, but ERCP can also be performed as an outpatient procedure, depending on the patient's condition and on the complexity of the required procedure.
ERCP Preparation
You will be asked not to eat or drink anything for six to eight hours before the test. It is important for the stomach to be empty to allow the endoscopist to visualize the entire area, and to decrease the chance of vomiting during the procedure.
ou may be instructed to adjust the dose of your medications or stop taking specific medications prior to the examination. Most drugs can be continued as usual, but some medications need to be discontinued for several days. All medications and dietary supplements should be discussed with your provider, since some are more important than others; for example, if you are taking a blood-thinning medication, the provider will determine how and when you should stop taking this prior to ERCP. If you are diabetic, adjustments will be made to your morning doses of medication (tablets or insulin) because you cannot eat anything before your ERCP.
If you are pregnant, the ERCP should be postponed until after childbirth if possible, but if the procedure is urgent, it can be done safely during pregnancy.
You will need a friend or family member to escort you home after the examination. This is because the medications used for sedation can impair reflexes, judgment, and your ability to drive (similar to the effects of alcohol).
What to Expect in the Endoscopy Unit
Prior to the endoscopy, you will be asked some questions about your medical history and the medications you are currently taking, and the results of your blood tests will be checked; the ERCP procedure will also be explained in detail, and the doctor will verify that the consent form was signed.
Sedation — The nurse will start an intravenous (IV) line (by inserting a needle into a vein in the hand or arm) to administer medications. Most endoscopy units use a combination of a sedative to induce relaxation, and a medication to prevent discomfort. This is called "conscious sedation" because you are awake, but the body is relaxed and pain is numbed. In some more complicated cases, you may be sedated more heavily or given anesthesia (put to sleep) for the ERCP.
For safety reasons, you will be asked to remove eyeglasses or contact lenses, and dentures. Before the procedure begins, you may be given local anesthetic (a numbing spray applied onto the throat or gargled).
ERCP Procedure
ERCP is performed in a room that contains X-ray equipment. You will lie on a special table during the examination, generally on your left side or stomach.
Although many people worry about discomfort from the endoscopy, most people tolerate it well and feel fine afterwards. Medications will be given through the IV line during the procedure. A plastic mouth guard is placed between the teeth to prevent damage to the teeth and endoscope. Many patients sleep during the test; others are very relaxed and not aware of the examination.
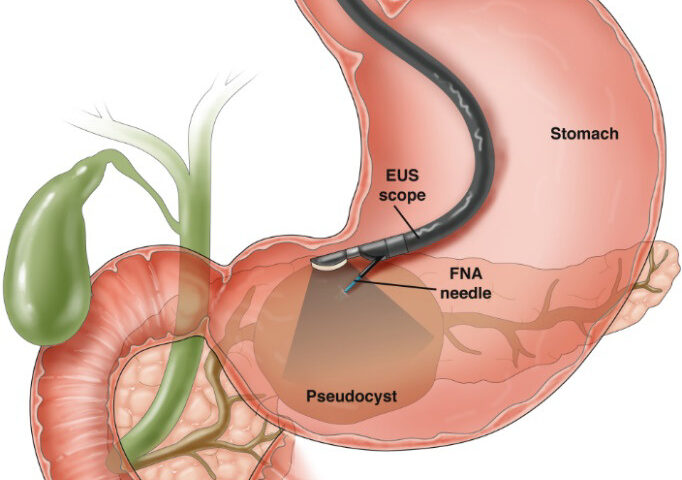
The ERCP endoscope is a special flexible tube, approximately the size of a finger. It contains a lens and a light source that allows the endoscopist to view the inside of the patient's body; images are magnified on a monitor so that even very small details and changes can be seen. The endoscope also contains channels that allow the endoscopist to take biopsies (painless tissue samples) and introduce or withdraw fluid, air, or other instruments.
You will be asked to swallow the tube; most people have no difficulty with this as a result of the sedating medications. Once the scope is inserted through the mouth, air is gently introduced to open up the esophagus, stomach, and intestine so the scope can be passed through those structures and to allow the endoscopist . A small plastic tube (cannula) is passed through the endoscope into the opening of the bile duct through a structure called the papilla, dye is injected, and X-ray pictures are taken after the injection and displayed on a TV monitor so the endoscopist can examine the bile ducts and pancreatic duct.
Depending on what the endoscopist sees during the ERCP, he or she may perform a variety of procedures or treatments. If bile duct stones are present in the common bile duct, the opening of the papilla can be widened by application of electrocautery , and the stones are removed, sometimes with the aid of a basket. If the X-ray pictures show a narrowing of the bile duct, a stent (a small wire-mesh or plastic tube) can be inserted to allow the bile to bypass the blockage and pass into the duodenum.
You may experience mild discomfort as air is introduced through the endoscope. This is not harmful and belching may relieve the sensation. The endoscope does not interfere with breathing. Taking slow and deep breaths during the procedure may help you to relax.
The length of the examination varies between 30 and 90 minutes (usually about an hour).
Recovery After ERCP
After ERCP, you will be monitored while the sedative medications wear off. The medicines cause most people to temporarily feel tired or have difficulty concentrating, so it is usually advised not to return to work or drive that day.
The most common discomfort after the examination is a feeling of bloating as a result of the air introduced during the examination. This usually resolves quickly. Some people also have a mild sore throat. Most people are able to drink clear liquids shortly after the examination. In some cases, blood tests may be done the same day following ERCP.
The endoscopist can usually tell the patient the results of their examination right away. If biopsies were taken, the tissue will need to be sent to a lab for analysis.
ERCP Complications
ERCP is a safe procedure and serious complications are uncommon. If complications do occur, they are usually mild, and may include the following:
- Pancreatitis (inflammation of the pancreas) is the most frequent complication, occurring in about 3 to 5 percent of people undergoing ERCP. When it occurs, it is usually mild, causing abdominal pain and nausea, which resolve after a few days in the hospital. Rarely pancreatitis may be more severe.
- Sometimes the endoscopist needs to make a cut into the ampulla (the place where the common bile duct and pancreatic duct join the small bowel). Bleeding can occur from a cut into the ampulla, but it is usually minimal and stops quickly by itself or can be controlled during the ERCP procedure. For patients on warfarin or other blood-thinning medication there is an increased risk of post-procedure bleeding compared with patients who do not take these medications.
- The ERCP scope or other instruments can cause a tear or hole in the intestine being examined (called perforation). This is a serious condition, often requiring surgical intervention, although it occurs rarely.
- Infection of the bile ducts (cholangitis) is rare in general, but it can occur, particularly in patients with certain preexisting conditions. Treatment of infections requires antibiotics and drainage of excess fluid.
- Aspiration (inhalation) of food or fluids into the lungs. The risk of this complication is minimal in people who do not eat or drink for several hours before the examination.
The following symptoms should be reported immediately:
- Severe abdominal pain (not just gas cramps)
- A firm, distended abdomen
- Vomiting
- Fever or chills
- Difficulty in swallowing or a severe sore throat
- A crunching feeling under the skin